1. What is the projected Compound Annual Growth Rate (CAGR) of the U.S. Pharmacy Benefit Management Market?
The projected CAGR is approximately 5.9%.
MR Forecast provides premium market intelligence on deep technologies that can cause a high level of disruption in the market within the next few years. When it comes to doing market viability analyses for technologies at very early phases of development, MR Forecast is second to none. What sets us apart is our set of market estimates based on secondary research data, which in turn gets validated through primary research by key companies in the target market and other stakeholders. It only covers technologies pertaining to Healthcare, IT, big data analysis, block chain technology, Artificial Intelligence (AI), Machine Learning (ML), Internet of Things (IoT), Energy & Power, Automobile, Agriculture, Electronics, Chemical & Materials, Machinery & Equipment's, Consumer Goods, and many others at MR Forecast. Market: The market section introduces the industry to readers, including an overview, business dynamics, competitive benchmarking, and firms' profiles. This enables readers to make decisions on market entry, expansion, and exit in certain nations, regions, or worldwide. Application: We give painstaking attention to the study of every product and technology, along with its use case and user categories, under our research solutions. From here on, the process delivers accurate market estimates and forecasts apart from the best and most meaningful insights.
Products generically come under this phrase and may imply any number of goods, components, materials, technology, or any combination thereof. Any business that wants to push an innovative agenda needs data on product definitions, pricing analysis, benchmarking and roadmaps on technology, demand analysis, and patents. Our research papers contain all that and much more in a depth that makes them incredibly actionable. Products broadly encompass a wide range of goods, components, materials, technologies, or any combination thereof. For businesses aiming to advance an innovative agenda, access to comprehensive data on product definitions, pricing analysis, benchmarking, technological roadmaps, demand analysis, and patents is essential. Our research papers provide in-depth insights into these areas and more, equipping organizations with actionable information that can drive strategic decision-making and enhance competitive positioning in the market.
 U.S. Pharmacy Benefit Management Market
U.S. Pharmacy Benefit Management MarketU.S. Pharmacy Benefit Management Market by Service (Specialty Pharmacy Services, Benefit Plan Design & Administration, Pharmacy Claims Processing, Formulary Management, Others), by Service Provider (Insurance Companies, Retail Pharmacies, Standalone PBMs), by Forecast 2026-2034
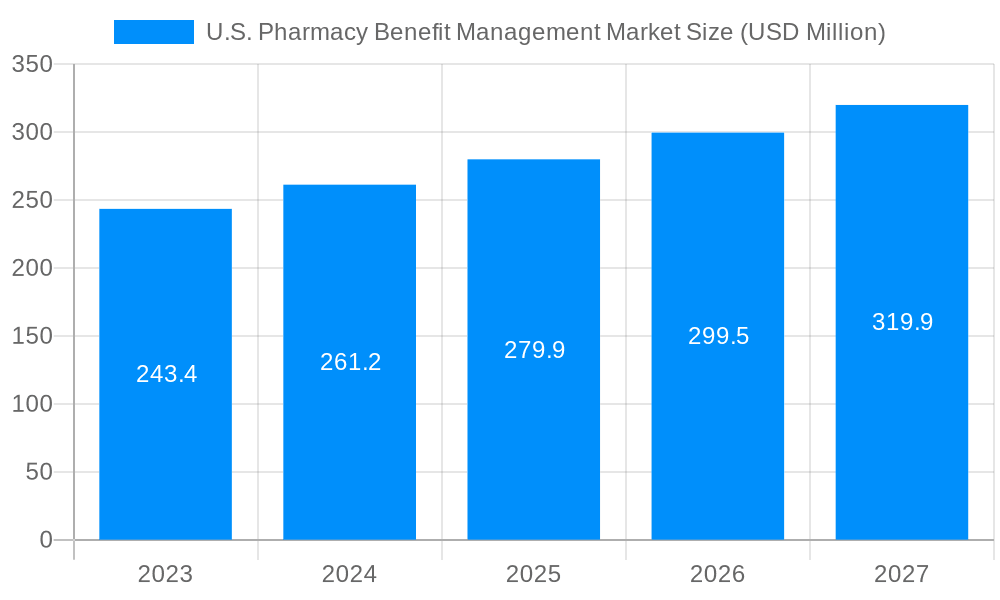
The U.S. Pharmacy Benefit Management Market size was valued at USD 498.5 USD Million in 2023 and is projected to reach USD 744.62 USD Million by 2032, exhibiting a CAGR of 5.9 % during the forecast period. Pharmacy Benefit Management (PBM), in other words, is the role of institutions responsible for the management of prescription drug programs for health insurance companies, employers, as well as government programs. PBMs do the following functions: negotiate drug costs with drug makers, process reimbursement claims, and control drug usage. The PBMs could be entities operating as stand-alone, PBMs implemented inside of health plans, or pharmacy chains that have PBM services. Main PBM components such as formulary management, proper usage of medication, and prescription networks are the most common. Along the same lines, PBMs are equipped with support services such as mail-order pharmacy and specialty pharmacy management. In the US, pharmacy benefit managers (PBMs) assume control over the costs of medications and patients, drug access is a necessity. Market trends currently existing in PBM US are characterized by a high level of consolidation of PBMs, the introduction of a value-based approach, and technology application for data analysis and medication adherence programs.



Service:
Service Provider:
| Aspects | Details |
|---|---|
| Study Period | 2020-2034 |
| Base Year | 2025 |
| Estimated Year | 2026 |
| Forecast Period | 2026-2034 |
| Historical Period | 2020-2025 |
| Growth Rate | CAGR of 5.9% from 2020-2034 |
| Segmentation |
|




Note*: In applicable scenarios
Primary Research
Secondary Research

Involves using different sources of information in order to increase the validity of a study
These sources are likely to be stakeholders in a program - participants, other researchers, program staff, other community members, and so on.
Then we put all data in single framework & apply various statistical tools to find out the dynamic on the market.
During the analysis stage, feedback from the stakeholder groups would be compared to determine areas of agreement as well as areas of divergence
The projected CAGR is approximately 5.9%.
Key companies in the market include CVS Health (U.S.), Cigna (U.S.), OptumRx, Inc. (U.S.), Anthem, Inc. (U.S.), Abarca Health LLC. (U.S.), Express Scripts (U.S.), Medimpact (U.S.), Walgreens Boots Alliance , Humana Pharmacy Solutions , Magellan Rx Management.
The market segments include Service, Service Provider.
The market size is estimated to be USD 498.5 USD Million as of 2022.
Introduction of Cost-effective Manufacturing Processes to Drive Market Growth.
Increasing Number of Hospitals and ASCs Identified as Significant Market Trend.
High Costs for Patients & Healthcare System by Pharmacy Benefit Managers to Hinder Market Growth.
November 2021 - Anthem, Inc. entered into an agreement to acquire Integra Managed Care to increase its network.
Pricing options include single-user, multi-user, and enterprise licenses priced at USD 2850, USD 3850, and USD 4850 respectively.
The market size is provided in terms of value, measured in USD Million.
Yes, the market keyword associated with the report is "U.S. Pharmacy Benefit Management Market," which aids in identifying and referencing the specific market segment covered.
The pricing options vary based on user requirements and access needs. Individual users may opt for single-user licenses, while businesses requiring broader access may choose multi-user or enterprise licenses for cost-effective access to the report.
While the report offers comprehensive insights, it's advisable to review the specific contents or supplementary materials provided to ascertain if additional resources or data are available.
To stay informed about further developments, trends, and reports in the U.S. Pharmacy Benefit Management Market, consider subscribing to industry newsletters, following relevant companies and organizations, or regularly checking reputable industry news sources and publications.