1. What is the projected Compound Annual Growth Rate (CAGR) of the Medical Payment Fraud Detection?
The projected CAGR is approximately XX%.
MR Forecast provides premium market intelligence on deep technologies that can cause a high level of disruption in the market within the next few years. When it comes to doing market viability analyses for technologies at very early phases of development, MR Forecast is second to none. What sets us apart is our set of market estimates based on secondary research data, which in turn gets validated through primary research by key companies in the target market and other stakeholders. It only covers technologies pertaining to Healthcare, IT, big data analysis, block chain technology, Artificial Intelligence (AI), Machine Learning (ML), Internet of Things (IoT), Energy & Power, Automobile, Agriculture, Electronics, Chemical & Materials, Machinery & Equipment's, Consumer Goods, and many others at MR Forecast. Market: The market section introduces the industry to readers, including an overview, business dynamics, competitive benchmarking, and firms' profiles. This enables readers to make decisions on market entry, expansion, and exit in certain nations, regions, or worldwide. Application: We give painstaking attention to the study of every product and technology, along with its use case and user categories, under our research solutions. From here on, the process delivers accurate market estimates and forecasts apart from the best and most meaningful insights.
Products generically come under this phrase and may imply any number of goods, components, materials, technology, or any combination thereof. Any business that wants to push an innovative agenda needs data on product definitions, pricing analysis, benchmarking and roadmaps on technology, demand analysis, and patents. Our research papers contain all that and much more in a depth that makes them incredibly actionable. Products broadly encompass a wide range of goods, components, materials, technologies, or any combination thereof. For businesses aiming to advance an innovative agenda, access to comprehensive data on product definitions, pricing analysis, benchmarking, technological roadmaps, demand analysis, and patents is essential. Our research papers provide in-depth insights into these areas and more, equipping organizations with actionable information that can drive strategic decision-making and enhance competitive positioning in the market.
 Medical Payment Fraud Detection
Medical Payment Fraud DetectionMedical Payment Fraud Detection by Type (/> On-premise, Cloud-based), by Application (/> Private Insurance Payers, Public/Government Agencies, Third-Party Service Providers), by North America (United States, Canada, Mexico), by South America (Brazil, Argentina, Rest of South America), by Europe (United Kingdom, Germany, France, Italy, Spain, Russia, Benelux, Nordics, Rest of Europe), by Middle East & Africa (Turkey, Israel, GCC, North Africa, South Africa, Rest of Middle East & Africa), by Asia Pacific (China, India, Japan, South Korea, ASEAN, Oceania, Rest of Asia Pacific) Forecast 2025-2033
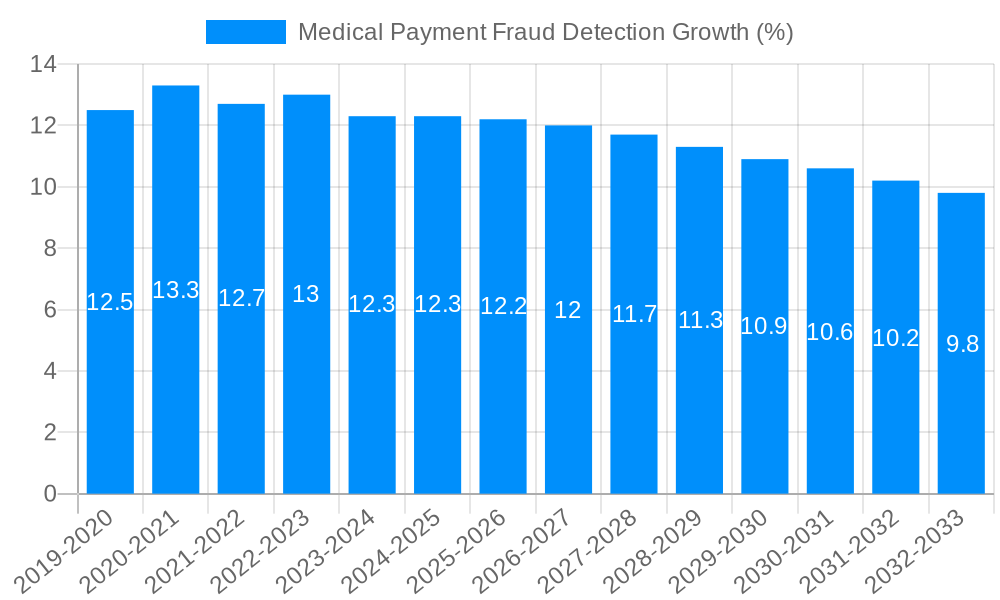
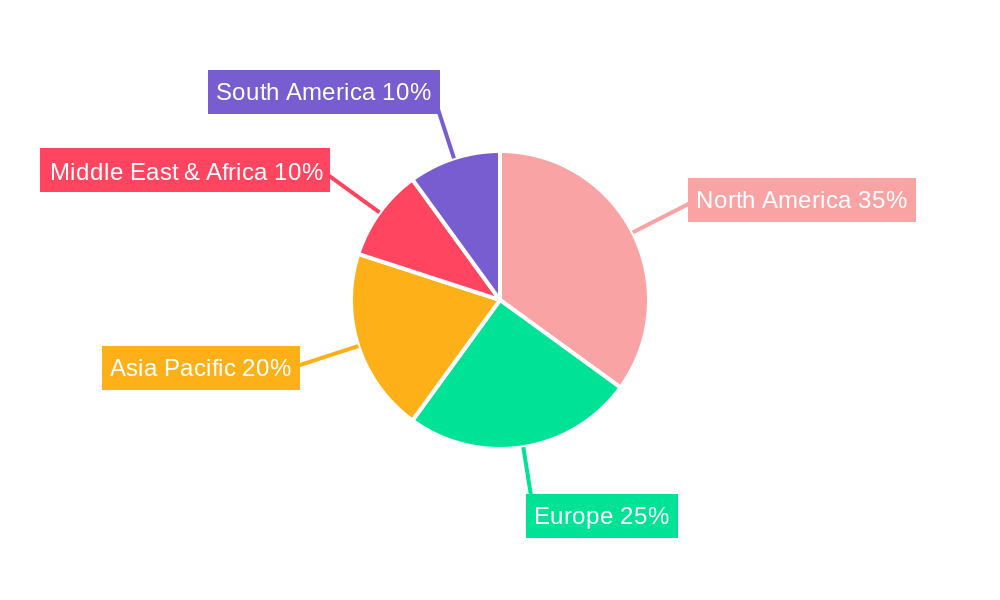
The medical payment fraud detection market is experiencing robust growth, driven by increasing healthcare expenditures, sophisticated fraud schemes, and a rising emphasis on regulatory compliance. The market, estimated at $15 billion in 2025, is projected to maintain a healthy Compound Annual Growth Rate (CAGR) of 12% from 2025 to 2033, reaching approximately $45 billion by 2033. This growth is fueled by the adoption of advanced analytics, machine learning, and artificial intelligence technologies to identify and prevent fraudulent claims. Key players like LexisNexis Risk Solutions, IBM, and Optuminsight are leveraging these technologies to provide comprehensive solutions that encompass data analysis, predictive modeling, and real-time fraud detection capabilities. The market is segmented by technology (rule-based systems, machine learning, AI), deployment mode (cloud, on-premises), and end-user (payers, providers). The North American region currently holds the largest market share due to advanced technological infrastructure and stringent regulatory frameworks. However, growth in emerging markets like Asia-Pacific is expected to accelerate, driven by increasing healthcare spending and government initiatives to combat fraud.
Significant restraints include the high cost of implementation and maintenance of sophisticated fraud detection systems, along with data privacy and security concerns. Overcoming these challenges requires collaborations between healthcare payers, providers, and technology vendors to develop efficient, secure, and cost-effective solutions. Future trends include the increasing adoption of blockchain technology for secure data management, integration with electronic health records (EHRs), and the development of more sophisticated predictive models to anticipate emerging fraud patterns. The market is expected to witness further consolidation as larger players acquire smaller companies to expand their product portfolios and market reach. The ongoing evolution of fraud techniques necessitates continuous innovation in fraud detection technologies to maintain effectiveness and safeguard the integrity of the healthcare system.
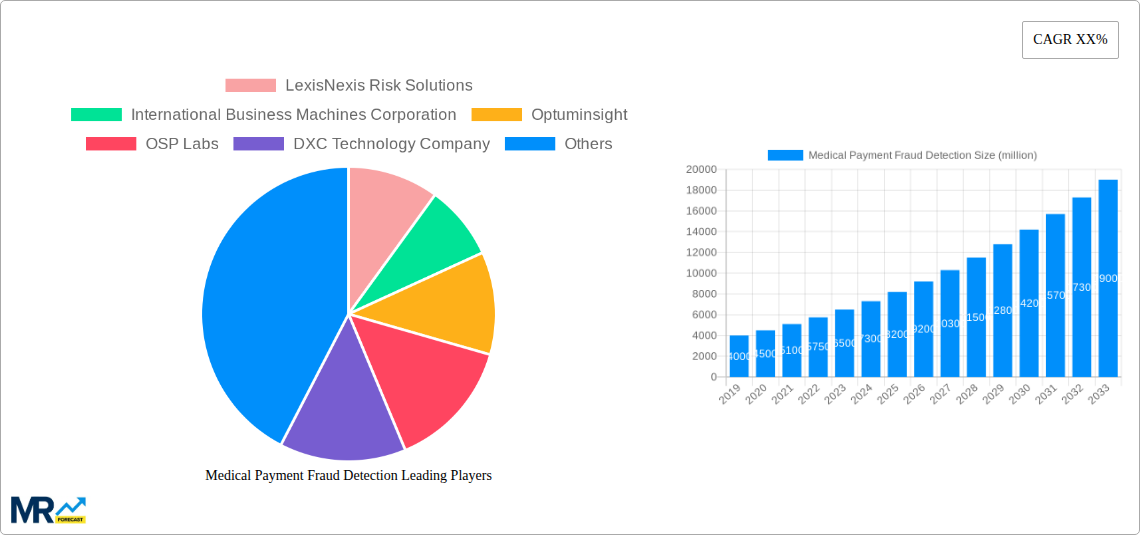
The medical payment fraud detection market is experiencing robust growth, projected to reach multi-billion dollar valuations by 2033. The study period, encompassing 2019-2033, reveals a significant upward trajectory, with the base year of 2025 serving as a pivotal point in this expansion. Key market insights indicate a strong correlation between rising healthcare expenditures and the increasing sophistication of fraudulent activities. This necessitates the adoption of advanced technologies and analytical tools for effective fraud detection. The estimated market value for 2025 already signals a substantial investment in this sector, reflecting a growing awareness of the financial and reputational risks associated with medical payment fraud. This trend is further fueled by stricter government regulations and increasing pressure on healthcare providers to demonstrate financial accountability. The forecast period, 2025-2033, anticipates continued growth driven by technological innovations, improved data analytics capabilities, and the evolving nature of fraudulent schemes. The historical period (2019-2024) showcases a gradual but steady increase in market size, laying the groundwork for the exponential growth predicted in the coming years. The market is witnessing a shift towards proactive fraud prevention strategies rather than solely reactive measures, indicating a more mature and sophisticated approach to risk management within the healthcare industry. This proactive approach involves leveraging predictive analytics, machine learning, and advanced data mining techniques to identify potential fraud risks before they materialize. This trend is significantly impacting the market’s growth, as organizations are increasingly willing to invest in preventative technologies that offer a higher return on investment than reactive measures. The market is also seeing increased demand for solutions that integrate seamlessly with existing healthcare IT infrastructure, streamlining data analysis and reducing operational complexities.
Several factors are propelling the growth of the medical payment fraud detection market. The escalating costs of healthcare globally are a primary driver, making healthcare providers and payers increasingly vulnerable to financial losses due to fraudulent activities. The increasing prevalence and complexity of fraud schemes, from billing inaccuracies to identity theft, necessitates the deployment of sophisticated detection systems. Technological advancements, such as artificial intelligence (AI) and machine learning (ML), are providing more effective and efficient fraud detection capabilities. These technologies are capable of analyzing vast amounts of data to identify patterns and anomalies indicative of fraudulent behavior, surpassing the capabilities of traditional methods. Furthermore, stricter government regulations and increased penalties for fraudulent activities are incentivizing healthcare organizations to invest in robust fraud detection solutions to mitigate risk and ensure compliance. The growing awareness among healthcare providers and payers regarding the financial and reputational consequences of undetected fraud is also contributing to the market's expansion. Finally, the rise of big data and advanced analytics empowers organizations to gain deeper insights into their data, leading to improved detection rates and reduced financial losses. The convergence of these factors is creating a robust market poised for sustained growth in the years to come.
Despite the considerable growth potential, the medical payment fraud detection market faces certain challenges. The high cost of implementing and maintaining advanced fraud detection systems can be a significant barrier to entry, particularly for smaller healthcare providers. The complexity of healthcare data and the need for specialized expertise to analyze it effectively present another hurdle. Data integration and interoperability issues across different healthcare systems can also hinder effective fraud detection. Moreover, the ever-evolving nature of fraud schemes necessitates continuous updates and improvements to detection systems, requiring ongoing investment and adaptation. Concerns regarding data privacy and security are also paramount, as handling sensitive patient information requires robust security measures to comply with regulations like HIPAA. Finally, a shortage of skilled professionals with expertise in data analytics and fraud detection can limit the effective implementation and utilization of these advanced systems. Addressing these challenges will be crucial for unlocking the full potential of the medical payment fraud detection market.
North America: This region is expected to hold a significant market share due to the high prevalence of healthcare fraud, advanced technological infrastructure, and a strong regulatory environment. The US, in particular, is a major market driver, with substantial investments in healthcare IT and data analytics.
Europe: The increasing adoption of electronic health records (EHRs) and stricter regulations are driving market growth in Europe. Countries like Germany and the UK are key contributors due to their developed healthcare systems and growing awareness of the need for robust fraud detection.
Asia Pacific: This region exhibits rapid growth potential, driven by increasing healthcare expenditure, government initiatives to combat fraud, and the adoption of advanced technologies. Countries like India and China are expected to witness significant market expansion.
Segments:
Solution Type: Software solutions are gaining popularity due to their scalability, flexibility, and cost-effectiveness. However, service offerings are also vital for ensuring proper implementation, training, and ongoing support. The market shows significant growth in both segments, suggesting a comprehensive approach to fraud prevention is increasingly valued.
Deployment Mode: Cloud-based deployments are becoming more prevalent due to their accessibility, scalability, and cost-effectiveness compared to on-premise solutions. However, on-premise solutions will retain a niche within organizations with stringent security requirements or those needing granular control over their data.
End User: Hospitals and healthcare providers form a significant market segment due to their high volume of transactions and vulnerability to fraud. Payers (insurance companies and government agencies) also represent a substantial segment, as they are responsible for reimbursing healthcare costs and need to prevent fraudulent claims.
The paragraph below summarizes the above. The North American market, particularly the US, is anticipated to lead due to high fraud incidents, technological advancements, and stringent regulations. Europe follows, fueled by EHR adoption and stronger regulations. The Asia-Pacific region exhibits high growth potential due to rising healthcare expenditure and technological adoption. Within segments, software solutions and cloud deployments dominate, while hospitals and payers are the key end-users. All segments showcase significant growth, reflecting a comprehensive market approach to fraud prevention and detection.
The increasing adoption of cloud-based solutions, the rising prevalence of big data analytics, and the implementation of advanced AI and machine learning algorithms are key growth catalysts. These technologies enhance the efficiency and effectiveness of fraud detection, leading to increased market demand. Furthermore, rising government regulations and the increasing awareness of the financial risks associated with medical payment fraud are driving organizations to invest heavily in these solutions.
This report provides a comprehensive overview of the medical payment fraud detection market, covering market size, growth trends, key drivers and restraints, competitive landscape, and future outlook. It offers invaluable insights for stakeholders across the healthcare ecosystem, including providers, payers, technology vendors, and regulatory bodies, enabling them to make informed strategic decisions in this rapidly evolving market.
| Aspects | Details |
|---|---|
| Study Period | 2019-2033 |
| Base Year | 2024 |
| Estimated Year | 2025 |
| Forecast Period | 2025-2033 |
| Historical Period | 2019-2024 |
| Growth Rate | CAGR of XX% from 2019-2033 |
| Segmentation |
|




Note*: In applicable scenarios
Primary Research
Secondary Research

Involves using different sources of information in order to increase the validity of a study
These sources are likely to be stakeholders in a program - participants, other researchers, program staff, other community members, and so on.
Then we put all data in single framework & apply various statistical tools to find out the dynamic on the market.
During the analysis stage, feedback from the stakeholder groups would be compared to determine areas of agreement as well as areas of divergence
The projected CAGR is approximately XX%.
Key companies in the market include LexisNexis Risk Solutions, International Business Machines Corporation, Optuminsight, OSP Labs, DXC Technology Company, Unitedhealth Group, SAS Institute, Fair Isaac Corporation, EXL Service Holdings, Inc., CGI GROUP, .
The market segments include Type, Application.
The market size is estimated to be USD XXX million as of 2022.
N/A
N/A
N/A
N/A
Pricing options include single-user, multi-user, and enterprise licenses priced at USD 4480.00, USD 6720.00, and USD 8960.00 respectively.
The market size is provided in terms of value, measured in million.
Yes, the market keyword associated with the report is "Medical Payment Fraud Detection," which aids in identifying and referencing the specific market segment covered.
The pricing options vary based on user requirements and access needs. Individual users may opt for single-user licenses, while businesses requiring broader access may choose multi-user or enterprise licenses for cost-effective access to the report.
While the report offers comprehensive insights, it's advisable to review the specific contents or supplementary materials provided to ascertain if additional resources or data are available.
To stay informed about further developments, trends, and reports in the Medical Payment Fraud Detection, consider subscribing to industry newsletters, following relevant companies and organizations, or regularly checking reputable industry news sources and publications.