1. What is the projected Compound Annual Growth Rate (CAGR) of the Healthcare Reimbursement?
The projected CAGR is approximately XX%.
MR Forecast provides premium market intelligence on deep technologies that can cause a high level of disruption in the market within the next few years. When it comes to doing market viability analyses for technologies at very early phases of development, MR Forecast is second to none. What sets us apart is our set of market estimates based on secondary research data, which in turn gets validated through primary research by key companies in the target market and other stakeholders. It only covers technologies pertaining to Healthcare, IT, big data analysis, block chain technology, Artificial Intelligence (AI), Machine Learning (ML), Internet of Things (IoT), Energy & Power, Automobile, Agriculture, Electronics, Chemical & Materials, Machinery & Equipment's, Consumer Goods, and many others at MR Forecast. Market: The market section introduces the industry to readers, including an overview, business dynamics, competitive benchmarking, and firms' profiles. This enables readers to make decisions on market entry, expansion, and exit in certain nations, regions, or worldwide. Application: We give painstaking attention to the study of every product and technology, along with its use case and user categories, under our research solutions. From here on, the process delivers accurate market estimates and forecasts apart from the best and most meaningful insights.
Products generically come under this phrase and may imply any number of goods, components, materials, technology, or any combination thereof. Any business that wants to push an innovative agenda needs data on product definitions, pricing analysis, benchmarking and roadmaps on technology, demand analysis, and patents. Our research papers contain all that and much more in a depth that makes them incredibly actionable. Products broadly encompass a wide range of goods, components, materials, technologies, or any combination thereof. For businesses aiming to advance an innovative agenda, access to comprehensive data on product definitions, pricing analysis, benchmarking, technological roadmaps, demand analysis, and patents is essential. Our research papers provide in-depth insights into these areas and more, equipping organizations with actionable information that can drive strategic decision-making and enhance competitive positioning in the market.
 Healthcare Reimbursement
Healthcare ReimbursementHealthcare Reimbursement by Application (/> Physician office, Hospitals, Diagnostic Laboratories, Others), by Type (/> Underpaid, Full Paid), by North America (United States, Canada, Mexico), by South America (Brazil, Argentina, Rest of South America), by Europe (United Kingdom, Germany, France, Italy, Spain, Russia, Benelux, Nordics, Rest of Europe), by Middle East & Africa (Turkey, Israel, GCC, North Africa, South Africa, Rest of Middle East & Africa), by Asia Pacific (China, India, Japan, South Korea, ASEAN, Oceania, Rest of Asia Pacific) Forecast 2025-2033
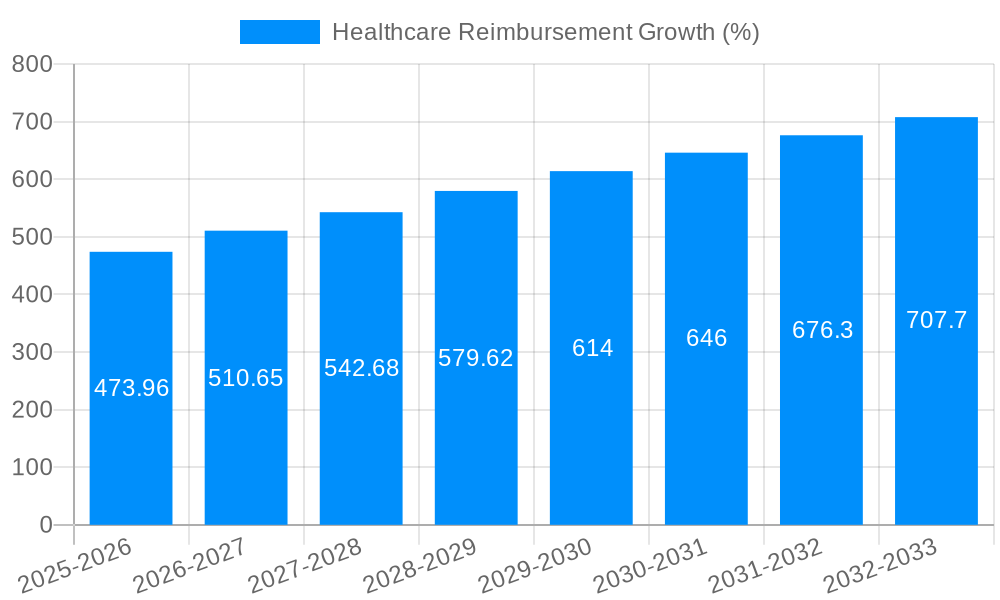
The global healthcare reimbursement market, valued at $8,479.11 million in 2025, is poised for substantial growth over the forecast period (2025-2033). While the exact CAGR is unavailable, considering the industry's ongoing expansion driven by factors like an aging global population, rising prevalence of chronic diseases, and increasing healthcare expenditure, a conservative estimate of 5-7% annual growth is plausible. This growth is fueled by the rising adoption of value-based care models, technological advancements in claims processing and payment systems, and a growing demand for greater transparency and efficiency in healthcare financing. Key players like UnitedHealth Group, Aetna, and Allianz are strategically investing in technological solutions and expanding their service offerings to capitalize on this market potential.
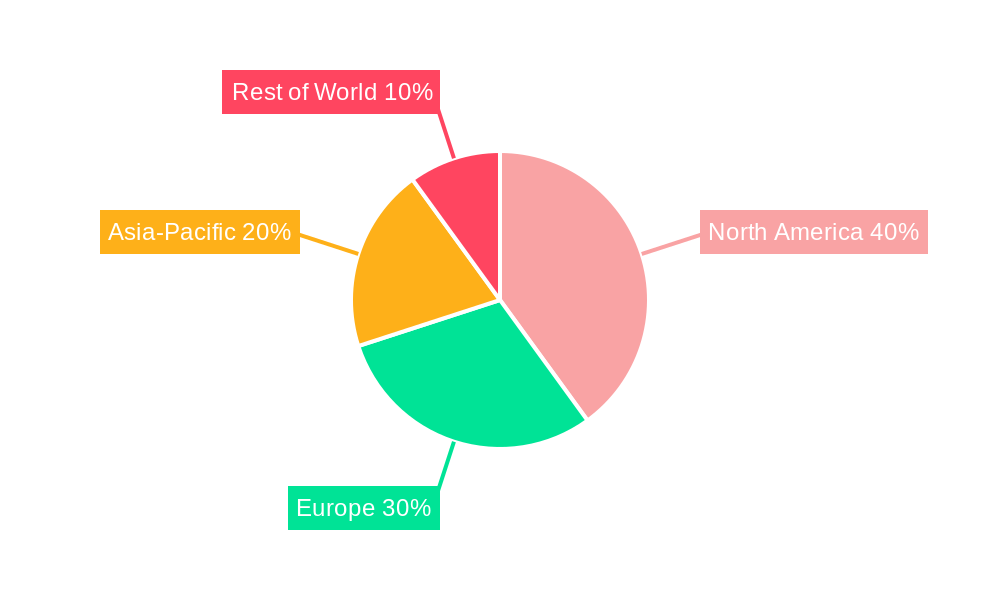
The market segmentation, though unspecified, likely includes various reimbursement methods (fee-for-service, capitation, bundled payments), payer types (private insurance, public insurance, self-pay), and healthcare services (hospital care, physician services, pharmaceuticals). Geographic variations are expected, with developed markets in North America and Europe leading the growth, followed by emerging economies in Asia-Pacific and Latin America. However, regulatory hurdles, varying reimbursement policies across countries, and data security concerns act as potential restraints, impacting overall market expansion. Future growth hinges on addressing these challenges, promoting interoperability between healthcare systems, and continuing the transition to more efficient and patient-centric models of care. The forecast period will witness increased focus on data analytics, artificial intelligence, and blockchain technology to enhance accuracy, reduce fraud, and streamline the reimbursement process.
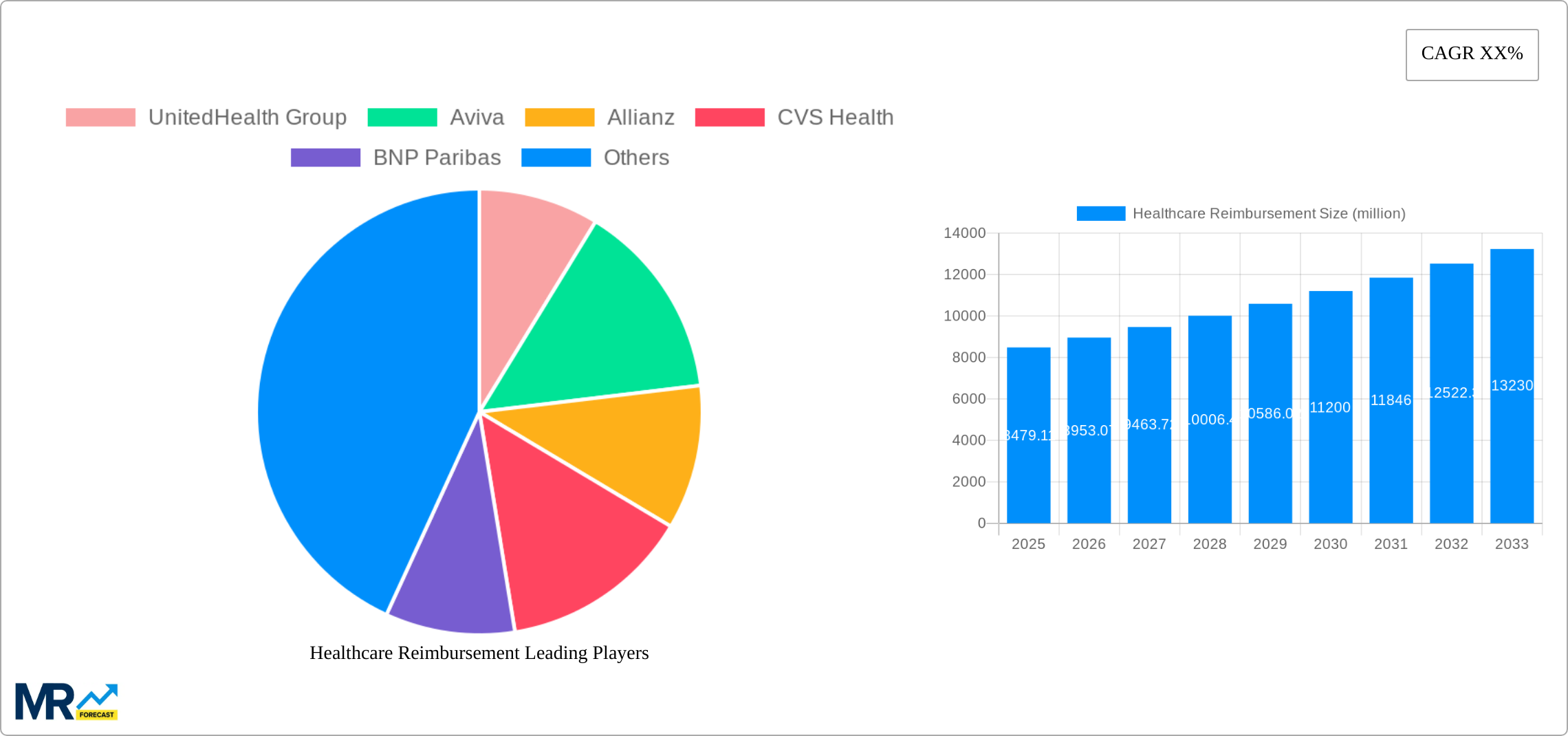
The global healthcare reimbursement market is experiencing a period of significant transformation, driven by a confluence of factors including technological advancements, evolving regulatory landscapes, and shifting consumer preferences. Over the study period (2019-2033), the market witnessed substantial growth, reaching an estimated value of XXX million in 2025. This growth is projected to continue throughout the forecast period (2025-2033), fueled by increasing healthcare expenditure globally and a rising prevalence of chronic diseases. The historical period (2019-2024) saw a steady increase in market size, setting the stage for the robust expansion anticipated in the coming years. Key market insights reveal a strong preference for value-based care models, increasing adoption of digital health technologies for claims processing and reimbursement, and the growing influence of data analytics in optimizing reimbursement strategies. The rise of telehealth and remote patient monitoring has also created new reimbursement pathways, impacting the traditional fee-for-service models. Furthermore, the increasing focus on population health management and preventive care is reshaping reimbursement structures, promoting incentives for improved patient outcomes. Competition among providers and payers is intensifying, driving innovation and efficiency in reimbursement processes. Regulatory changes across various regions are playing a crucial role, with governments striving to balance affordability, accessibility, and quality of care. This dynamic interplay of factors suggests a continuous evolution of the healthcare reimbursement landscape, presenting both opportunities and challenges for stakeholders across the value chain. The market's trajectory is expected to be significantly influenced by the success of ongoing initiatives to improve healthcare data interoperability and the widespread adoption of blockchain technology for secure and transparent transactions.
Several key factors are propelling the growth of the healthcare reimbursement market. The escalating prevalence of chronic diseases such as diabetes, cardiovascular ailments, and cancer necessitates increased healthcare spending, directly impacting reimbursement needs. The aging global population, with its associated rise in healthcare requirements, further fuels market expansion. Technological advancements, particularly in areas like telemedicine and big data analytics, are streamlining reimbursement processes, boosting efficiency, and reducing administrative costs. Government initiatives focused on improving healthcare access and affordability, often involving reforms in reimbursement policies, are also contributing significantly. The increasing adoption of value-based care models, shifting the focus from volume to value, is changing how healthcare services are reimbursed, emphasizing quality outcomes over the number of procedures. Moreover, the growing awareness among consumers regarding their healthcare rights and the increasing demand for transparency in healthcare costs are influencing reimbursement practices. These factors collectively drive the significant and sustained growth trajectory observed in the healthcare reimbursement market.
Despite the promising growth outlook, the healthcare reimbursement market faces several challenges. Data security and privacy concerns are paramount, particularly with the increasing reliance on digital technologies and the exchange of sensitive patient information. The complexity of reimbursement processes, involving various stakeholders and intricate regulations, poses significant hurdles to efficiency and timely payments. The lack of standardization in healthcare data formats and interoperability issues across different systems can create significant delays and inefficiencies. Fraud and abuse remain persistent threats, requiring robust compliance measures and continuous monitoring. The rising costs of healthcare services, coupled with evolving reimbursement policies, create pressure on both providers and payers to manage expenses effectively. Furthermore, disparities in healthcare access and affordability, particularly in underserved populations, pose a significant challenge to the equitable distribution of healthcare resources. Addressing these challenges requires collaborative efforts from all stakeholders to enhance transparency, streamline processes, and ensure fair and efficient healthcare reimbursement systems.
The North American region, particularly the United States, is expected to maintain its dominant position in the healthcare reimbursement market due to high healthcare expenditure, advanced healthcare infrastructure, and a large insured population. The European market is also anticipated to witness significant growth, driven by increasing healthcare spending and the implementation of various healthcare reforms. Within the segments, the hospital segment is likely to hold a substantial market share, given its crucial role in delivering a wide range of healthcare services. However, the outpatient segment is also expected to experience considerable growth, fueled by the increasing popularity of ambulatory care settings and the rising adoption of telehealth services. The physician segment plays a pivotal role, representing a significant portion of healthcare spending.
The Asia-Pacific region is projected to exhibit significant growth potential due to rapid economic development, rising healthcare awareness, and government initiatives aimed at improving healthcare infrastructure. However, regulatory hurdles and varying levels of healthcare infrastructure across the region will influence market penetration.
The healthcare reimbursement market is propelled by several key growth catalysts. Technological advancements like AI-powered claims processing and blockchain for secure transactions are significantly enhancing efficiency and transparency. The increasing adoption of value-based care models incentivizes improved patient outcomes and cost-effective solutions. Government regulations supporting interoperability and data standardization are fostering a more seamless and efficient reimbursement ecosystem. Finally, rising consumer demand for personalized healthcare experiences is driving the development of innovative reimbursement strategies and technologies tailored to individual needs.
This report provides a comprehensive analysis of the healthcare reimbursement market, encompassing historical data, current market trends, and future projections. It offers insights into key driving forces, challenges, and growth opportunities, along with detailed profiles of leading market players. The report also provides regional and segment-specific analyses, offering a granular perspective on market dynamics. This detailed analysis equips stakeholders with the necessary information to make informed strategic decisions in this dynamic and evolving market.
| Aspects | Details |
|---|---|
| Study Period | 2019-2033 |
| Base Year | 2024 |
| Estimated Year | 2025 |
| Forecast Period | 2025-2033 |
| Historical Period | 2019-2024 |
| Growth Rate | CAGR of XX% from 2019-2033 |
| Segmentation |
|




Note*: In applicable scenarios
Primary Research
Secondary Research

Involves using different sources of information in order to increase the validity of a study
These sources are likely to be stakeholders in a program - participants, other researchers, program staff, other community members, and so on.
Then we put all data in single framework & apply various statistical tools to find out the dynamic on the market.
During the analysis stage, feedback from the stakeholder groups would be compared to determine areas of agreement as well as areas of divergence
The projected CAGR is approximately XX%.
Key companies in the market include UnitedHealth Group, Aviva, Allianz, CVS Health, BNP Paribas, Aetna, Nippon Life Insurance, WellCare Health Plans, AgileHealthInsurance, The Blue Cross Blue Shield Association.
The market segments include Application, Type.
The market size is estimated to be USD 8479110 million as of 2022.
N/A
N/A
N/A
N/A
Pricing options include single-user, multi-user, and enterprise licenses priced at USD 4480.00, USD 6720.00, and USD 8960.00 respectively.
The market size is provided in terms of value, measured in million.
Yes, the market keyword associated with the report is "Healthcare Reimbursement," which aids in identifying and referencing the specific market segment covered.
The pricing options vary based on user requirements and access needs. Individual users may opt for single-user licenses, while businesses requiring broader access may choose multi-user or enterprise licenses for cost-effective access to the report.
While the report offers comprehensive insights, it's advisable to review the specific contents or supplementary materials provided to ascertain if additional resources or data are available.
To stay informed about further developments, trends, and reports in the Healthcare Reimbursement, consider subscribing to industry newsletters, following relevant companies and organizations, or regularly checking reputable industry news sources and publications.