1. What is the projected Compound Annual Growth Rate (CAGR) of the DIPMedical Insurance Fee Control Management System?
The projected CAGR is approximately XX%.
MR Forecast provides premium market intelligence on deep technologies that can cause a high level of disruption in the market within the next few years. When it comes to doing market viability analyses for technologies at very early phases of development, MR Forecast is second to none. What sets us apart is our set of market estimates based on secondary research data, which in turn gets validated through primary research by key companies in the target market and other stakeholders. It only covers technologies pertaining to Healthcare, IT, big data analysis, block chain technology, Artificial Intelligence (AI), Machine Learning (ML), Internet of Things (IoT), Energy & Power, Automobile, Agriculture, Electronics, Chemical & Materials, Machinery & Equipment's, Consumer Goods, and many others at MR Forecast. Market: The market section introduces the industry to readers, including an overview, business dynamics, competitive benchmarking, and firms' profiles. This enables readers to make decisions on market entry, expansion, and exit in certain nations, regions, or worldwide. Application: We give painstaking attention to the study of every product and technology, along with its use case and user categories, under our research solutions. From here on, the process delivers accurate market estimates and forecasts apart from the best and most meaningful insights.
Products generically come under this phrase and may imply any number of goods, components, materials, technology, or any combination thereof. Any business that wants to push an innovative agenda needs data on product definitions, pricing analysis, benchmarking and roadmaps on technology, demand analysis, and patents. Our research papers contain all that and much more in a depth that makes them incredibly actionable. Products broadly encompass a wide range of goods, components, materials, technologies, or any combination thereof. For businesses aiming to advance an innovative agenda, access to comprehensive data on product definitions, pricing analysis, benchmarking, technological roadmaps, demand analysis, and patents is essential. Our research papers provide in-depth insights into these areas and more, equipping organizations with actionable information that can drive strategic decision-making and enhance competitive positioning in the market.
 DIPMedical Insurance Fee Control Management System
DIPMedical Insurance Fee Control Management SystemDIPMedical Insurance Fee Control Management System by Type (On-premises, Cloud-based), by Application (Hospital, Clinic, Others), by North America (United States, Canada, Mexico), by South America (Brazil, Argentina, Rest of South America), by Europe (United Kingdom, Germany, France, Italy, Spain, Russia, Benelux, Nordics, Rest of Europe), by Middle East & Africa (Turkey, Israel, GCC, North Africa, South Africa, Rest of Middle East & Africa), by Asia Pacific (China, India, Japan, South Korea, ASEAN, Oceania, Rest of Asia Pacific) Forecast 2025-2033
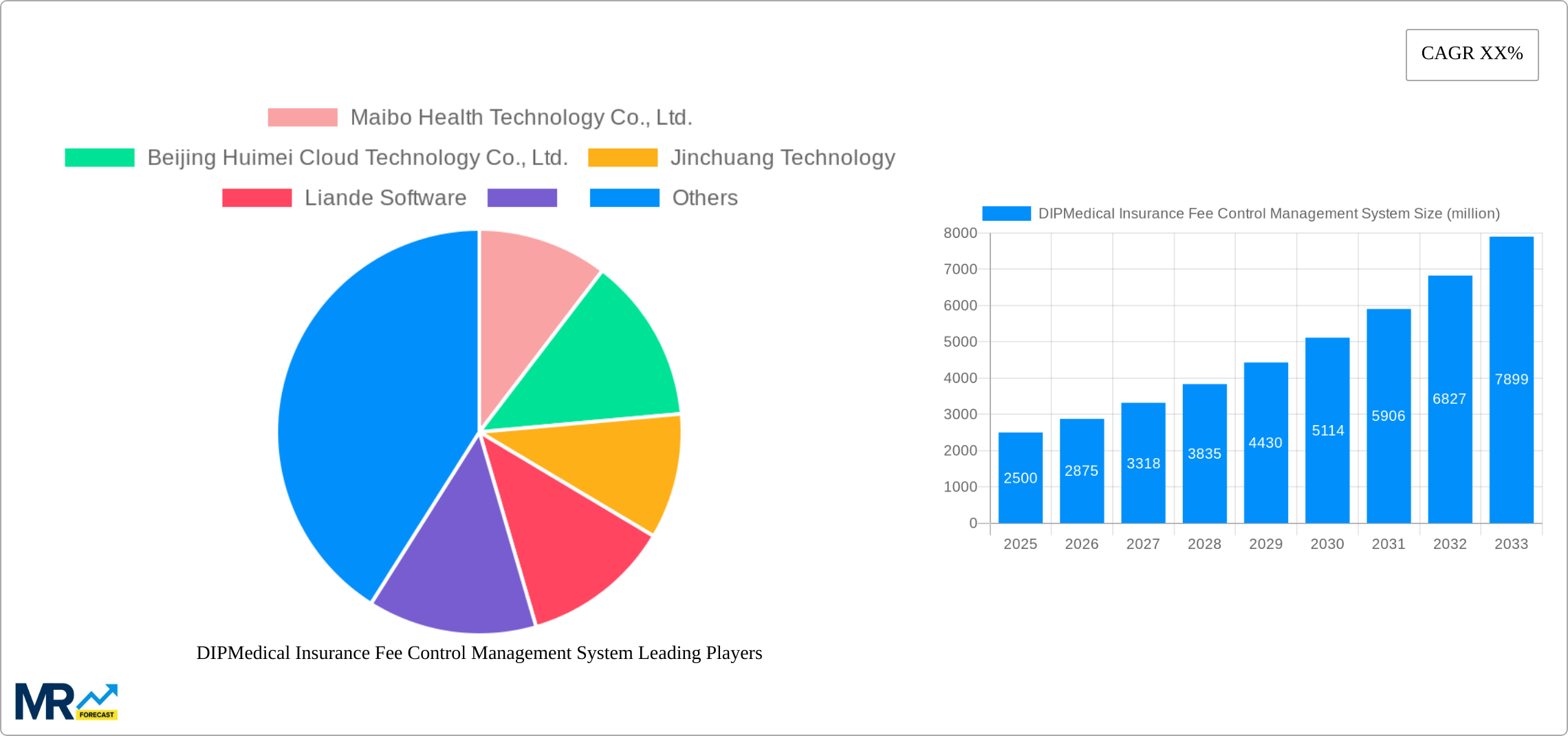
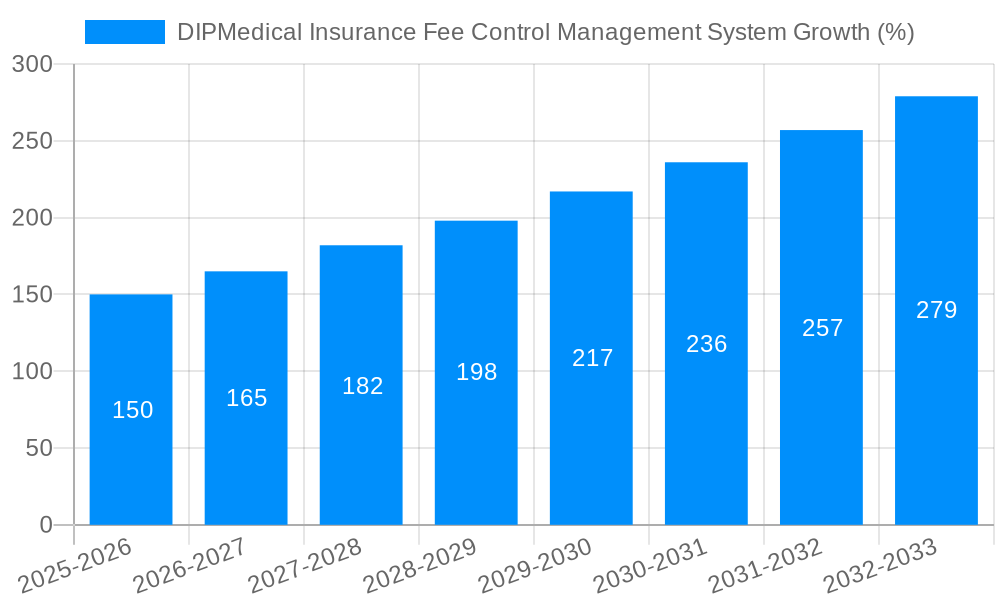
The DIP Medical Insurance Fee Control Management System market is experiencing robust growth, driven by increasing healthcare costs, stringent regulatory compliance requirements, and the rising adoption of digital health technologies. The market size in 2025 is estimated at $2.5 billion, projecting a Compound Annual Growth Rate (CAGR) of 15% from 2025 to 2033. This growth is fueled by several key factors. Firstly, governments worldwide are increasingly focusing on controlling healthcare expenditure, creating a significant demand for efficient fee management systems. Secondly, the shift towards cloud-based solutions offers scalability, improved data security, and reduced infrastructure costs, further accelerating market adoption. Finally, the increasing prevalence of chronic diseases and an aging global population contribute to higher healthcare utilization, making effective fee control systems essential.
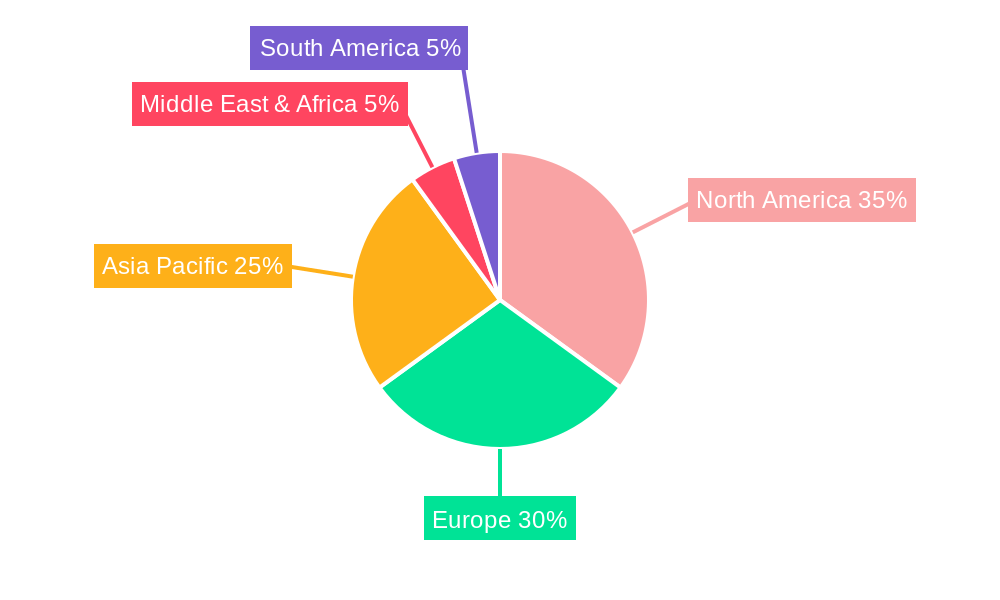
The market is segmented by deployment type (on-premises and cloud-based) and application (hospital, clinic, and others). The cloud-based segment is expected to dominate due to its inherent advantages. Geographically, North America and Europe currently hold significant market shares, driven by advanced healthcare infrastructure and regulatory frameworks. However, the Asia Pacific region is poised for substantial growth, fueled by increasing healthcare investments and expanding digitalization initiatives in countries like China and India. While the market faces challenges such as high initial implementation costs and data security concerns, the overall growth trajectory remains positive, indicating a promising outlook for vendors specializing in DIP Medical Insurance Fee Control Management Systems. Competition in this space is moderate, with established players focusing on innovation and strategic partnerships to strengthen their market positions.
The DIPMedical Insurance Fee Control Management System market is experiencing robust growth, projected to reach several billion USD by 2033. This surge is driven by a confluence of factors, including escalating healthcare costs, the increasing adoption of electronic health records (EHRs), and stringent government regulations aimed at improving healthcare efficiency and transparency. The historical period (2019-2024) witnessed a steady rise in market value, setting the stage for the impressive growth predicted during the forecast period (2025-2033). The base year of 2025 reveals a market already exceeding a significant milestone, with millions of USD in revenue, highlighting the system's established presence and growing importance within the healthcare sector. Key market insights include the shifting preference towards cloud-based solutions due to their scalability and cost-effectiveness, and a significant demand from hospitals, which constitute a large portion of the market. Further analysis indicates a strong correlation between technological advancements in data analytics and the expanding capabilities of DIPMedical Insurance Fee Control Management Systems. These systems are no longer simply cost-control mechanisms; they are evolving into sophisticated platforms capable of providing real-time insights into healthcare spending, enabling better resource allocation and strategic decision-making. The integration of artificial intelligence (AI) and machine learning (ML) is another key trend, with these technologies enhancing the accuracy and efficiency of fee control processes. The competitive landscape is characterized by both established players and emerging innovators, leading to a dynamic market with continuous product development and innovation. Finally, the increasing emphasis on value-based care is further fueling market expansion, as these systems are crucial for monitoring and managing the cost-effectiveness of healthcare services.
Several key factors are propelling the growth of the DIPMedical Insurance Fee Control Management System market. Firstly, the ever-increasing healthcare costs globally necessitate efficient systems for managing insurance fees. Governments and insurance providers are actively seeking solutions to curb escalating expenses, making DIPMedical systems a crucial investment. Secondly, the rising adoption of electronic health records (EHRs) creates a synergistic effect, facilitating seamless data integration and automation within the fee control process. The availability of structured data enhances accuracy and significantly reduces manual processing times. Thirdly, the implementation of stringent government regulations aimed at promoting transparency and accountability in healthcare billing practices is driving demand for compliance-oriented systems like DIPMedical. These regulations often mandate the use of specialized software for accurate claim processing and fraud detection. Furthermore, the increasing pressure on healthcare providers to improve efficiency and optimize resource allocation makes the use of these systems a strategic imperative. The systems offer real-time insights into spending patterns, empowering providers to make data-driven decisions regarding resource allocation and cost optimization. Finally, the growing adoption of value-based care models, which emphasize quality over quantity, requires meticulous tracking of healthcare costs and outcomes, thus increasing the demand for sophisticated fee control management systems.
Despite the promising growth trajectory, the DIPMedical Insurance Fee Control Management System market faces several challenges. One major hurdle is the high initial investment required for implementation and integration, particularly for smaller healthcare providers with limited budgets. This cost barrier can be a significant deterrent to adoption, especially in resource-constrained settings. Another significant challenge is the complexity of integrating these systems with existing legacy systems, often requiring significant time and resources for seamless data exchange. Data security and privacy concerns are also paramount, necessitating robust security measures to protect sensitive patient and financial information. This necessitates compliance with stringent data protection regulations, such as HIPAA in the US, adding to the overall cost and complexity. Furthermore, the continuous evolution of healthcare regulations and billing practices can render existing systems outdated, requiring regular updates and upgrades, which can be expensive and time-consuming. The shortage of skilled professionals proficient in implementing and managing these sophisticated systems also presents a significant challenge, limiting the widespread adoption and effective utilization of the technology. Finally, ensuring user adoption and training across various healthcare stakeholders can be a considerable hurdle, demanding effective change management strategies to successfully integrate the new system into existing workflows.
The hospital segment is expected to dominate the DIPMedical Insurance Fee Control Management System market throughout the forecast period (2025-2033). Hospitals, due to their scale and complex billing processes, stand to benefit the most from the automation and efficiency improvements offered by these systems. The high volume of claims processed daily necessitates sophisticated solutions to manage costs and ensure compliance.
Hospitals: The increasing complexity of hospital billing and the growing volume of patient data make automated fee control systems crucial for managing costs and ensuring compliance with regulations. The market within this segment is projected to reach hundreds of millions of USD by 2033. The adoption of sophisticated analytical tools within hospital settings is pushing demand for advanced DIPMedical systems capable of providing real-time insights into spending patterns and identifying areas for cost optimization. This has driven significant investments in infrastructure and training to support the adoption of these advanced systems.
Cloud-based solutions: Cloud-based systems offer significant advantages over on-premises solutions, including scalability, cost-effectiveness, and accessibility. Their ability to seamlessly integrate with existing EHRs and other hospital systems further enhances their appeal. The cloud-based market within the DIPMedical segment is projected to exhibit the highest growth rate during the forecast period. The flexibility and scalability of cloud-based systems particularly appeal to hospitals of varying sizes, making them a preferable choice over on-premises systems that require significant upfront investments.
Geographic Dominance: Developed economies like the United States and several European countries are expected to hold a substantial share of the market, driven by higher healthcare expenditures and advanced technological infrastructure. However, rapidly developing economies in Asia-Pacific are poised to witness significant growth due to increasing healthcare investment and rising adoption rates of technology in the healthcare sector. The adoption rates in these developing economies are accelerating, largely driven by government initiatives to improve healthcare efficiency and reduce healthcare costs. Specific countries in the Asia-Pacific region such as China, India, and South Korea are set to experience a significant rise in market share over the next decade.
The combination of these factors—high demand from hospitals, the growing popularity of cloud-based solutions, and robust growth in certain regions—paints a picture of a vibrant and rapidly expanding market for DIPMedical Insurance Fee Control Management Systems. The market's projected growth trajectory indicates significant opportunities for both established and emerging players in the years to come.
The DIPMedical Insurance Fee Control Management System industry's growth is fueled by several key catalysts. Government regulations emphasizing transparency and accountability in healthcare billing are driving adoption, while the increasing integration of these systems with EHRs streamlines processes and improves accuracy. Furthermore, the shift towards value-based care necessitates precise cost tracking and management, and advancements in data analytics provide valuable insights for cost optimization. The ongoing trend of digital transformation within the healthcare sector, coupled with the increasing adoption of cloud-based solutions, further accelerates market expansion.
This report offers a comprehensive analysis of the DIPMedical Insurance Fee Control Management System market, including detailed market sizing, growth projections, and key trend identification. It provides insights into the competitive landscape, identifying leading players and their strategies, as well as a thorough examination of the key driving factors, challenges, and growth catalysts shaping the industry. The report also offers a detailed segment analysis, covering various deployment types and applications, providing valuable information for stakeholders interested in understanding this dynamic market.
| Aspects | Details |
|---|---|
| Study Period | 2019-2033 |
| Base Year | 2024 |
| Estimated Year | 2025 |
| Forecast Period | 2025-2033 |
| Historical Period | 2019-2024 |
| Growth Rate | CAGR of XX% from 2019-2033 |
| Segmentation |
|




Note*: In applicable scenarios
Primary Research
Secondary Research

Involves using different sources of information in order to increase the validity of a study
These sources are likely to be stakeholders in a program - participants, other researchers, program staff, other community members, and so on.
Then we put all data in single framework & apply various statistical tools to find out the dynamic on the market.
During the analysis stage, feedback from the stakeholder groups would be compared to determine areas of agreement as well as areas of divergence
The projected CAGR is approximately XX%.
Key companies in the market include Maibo Health Technology Co., Ltd., Beijing Huimei Cloud Technology Co., Ltd., Jinchuang Technology, Liande Software, .
The market segments include Type, Application.
The market size is estimated to be USD XXX million as of 2022.
N/A
N/A
N/A
N/A
Pricing options include single-user, multi-user, and enterprise licenses priced at USD 4480.00, USD 6720.00, and USD 8960.00 respectively.
The market size is provided in terms of value, measured in million.
Yes, the market keyword associated with the report is "DIPMedical Insurance Fee Control Management System," which aids in identifying and referencing the specific market segment covered.
The pricing options vary based on user requirements and access needs. Individual users may opt for single-user licenses, while businesses requiring broader access may choose multi-user or enterprise licenses for cost-effective access to the report.
While the report offers comprehensive insights, it's advisable to review the specific contents or supplementary materials provided to ascertain if additional resources or data are available.
To stay informed about further developments, trends, and reports in the DIPMedical Insurance Fee Control Management System, consider subscribing to industry newsletters, following relevant companies and organizations, or regularly checking reputable industry news sources and publications.