1. What is the projected Compound Annual Growth Rate (CAGR) of the Provider Data Management Solution?
The projected CAGR is approximately 5%.
 Provider Data Management Solution
Provider Data Management SolutionProvider Data Management Solution by Type (Cloud Based, Web Based), by Application (Large Enterprises, SMEs), by North America (United States, Canada, Mexico), by South America (Brazil, Argentina, Rest of South America), by Europe (United Kingdom, Germany, France, Italy, Spain, Russia, Benelux, Nordics, Rest of Europe), by Middle East & Africa (Turkey, Israel, GCC, North Africa, South Africa, Rest of Middle East & Africa), by Asia Pacific (China, India, Japan, South Korea, ASEAN, Oceania, Rest of Asia Pacific) Forecast 2026-2034
MR Forecast provides premium market intelligence on deep technologies that can cause a high level of disruption in the market within the next few years. When it comes to doing market viability analyses for technologies at very early phases of development, MR Forecast is second to none. What sets us apart is our set of market estimates based on secondary research data, which in turn gets validated through primary research by key companies in the target market and other stakeholders. It only covers technologies pertaining to Healthcare, IT, big data analysis, block chain technology, Artificial Intelligence (AI), Machine Learning (ML), Internet of Things (IoT), Energy & Power, Automobile, Agriculture, Electronics, Chemical & Materials, Machinery & Equipment's, Consumer Goods, and many others at MR Forecast. Market: The market section introduces the industry to readers, including an overview, business dynamics, competitive benchmarking, and firms' profiles. This enables readers to make decisions on market entry, expansion, and exit in certain nations, regions, or worldwide. Application: We give painstaking attention to the study of every product and technology, along with its use case and user categories, under our research solutions. From here on, the process delivers accurate market estimates and forecasts apart from the best and most meaningful insights.
Products generically come under this phrase and may imply any number of goods, components, materials, technology, or any combination thereof. Any business that wants to push an innovative agenda needs data on product definitions, pricing analysis, benchmarking and roadmaps on technology, demand analysis, and patents. Our research papers contain all that and much more in a depth that makes them incredibly actionable. Products broadly encompass a wide range of goods, components, materials, technologies, or any combination thereof. For businesses aiming to advance an innovative agenda, access to comprehensive data on product definitions, pricing analysis, benchmarking, technological roadmaps, demand analysis, and patents is essential. Our research papers provide in-depth insights into these areas and more, equipping organizations with actionable information that can drive strategic decision-making and enhance competitive positioning in the market.
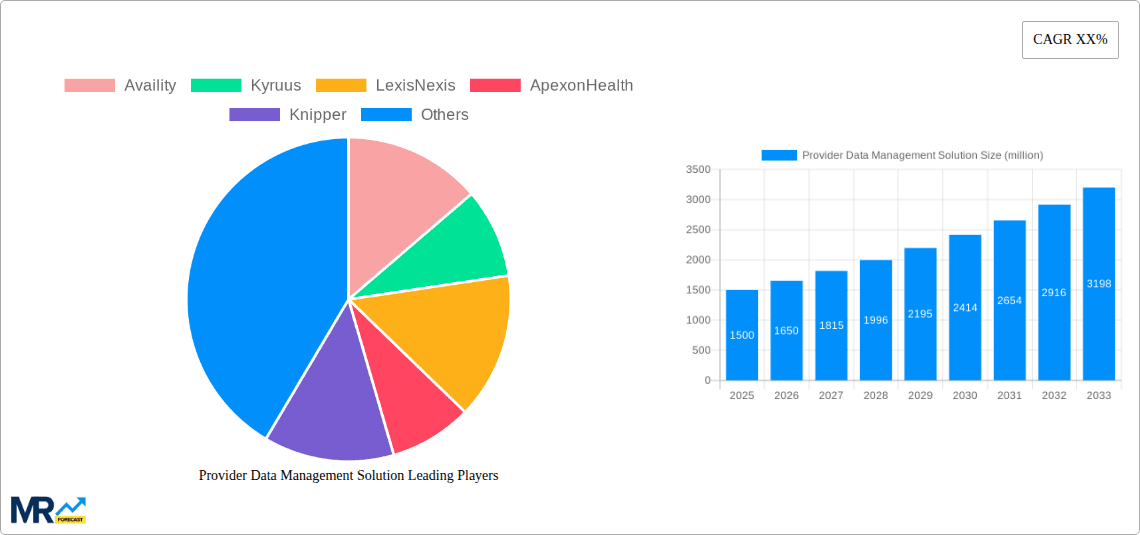
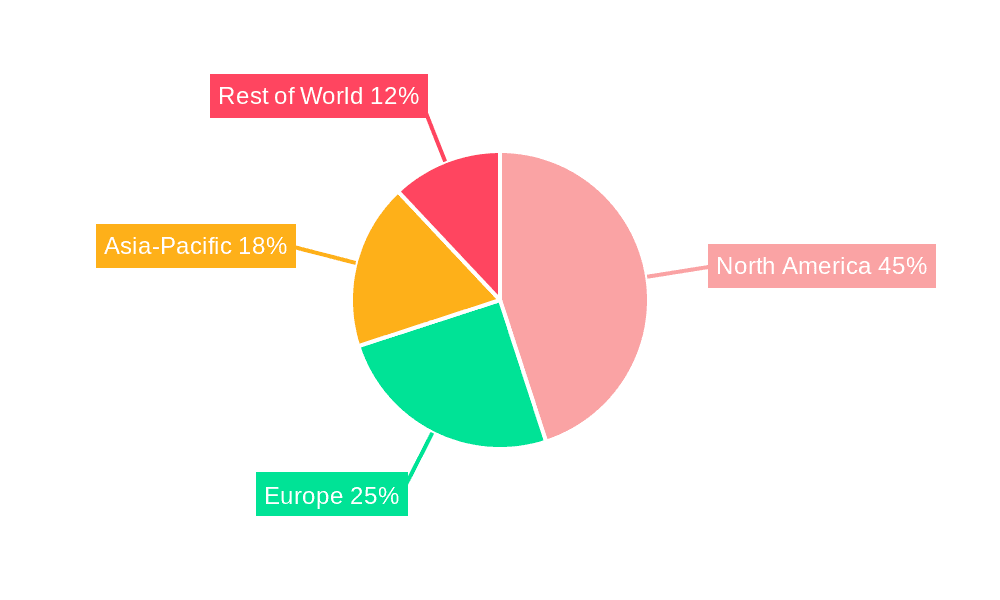
The Provider Data Management (PDM) solution market is experiencing robust growth, projected to reach $1012 million in 2025 and exhibiting a Compound Annual Growth Rate (CAGR) of 5% from 2025 to 2033. This expansion is fueled by several key drivers. The increasing complexity of healthcare regulations necessitates accurate and up-to-date provider data, driving demand for robust PDM solutions. Furthermore, the rising adoption of value-based care models requires efficient data management to optimize care coordination and reduce administrative burdens. The shift towards cloud-based solutions offers scalability and accessibility, contributing to market growth. Large enterprises and SMEs alike are adopting PDM solutions, reflecting the broad applicability across healthcare organizations of varying sizes. Competition is fierce, with established players like Availity, Kyruus, and LexisNexis alongside emerging companies like Simplify Healthcare and NextGate vying for market share. Geographic growth is anticipated across all regions, with North America currently holding a significant share due to advanced healthcare infrastructure and regulatory environments; however, Asia-Pacific and other emerging markets are poised for accelerated growth in the coming years as healthcare systems modernize and adopt digital technologies. The market segmentation by deployment (cloud-based and web-based) and user type (large enterprises and SMEs) provides avenues for tailored product offerings and strategic market penetration.

Continued growth in the PDM market will be influenced by factors such as advancements in data analytics and artificial intelligence (AI). These technologies enhance the capabilities of PDM solutions, allowing for predictive analytics, improved data quality, and streamlined workflows. However, challenges such as data security concerns, integration complexities with existing healthcare IT systems, and the high cost of implementation could potentially restrain market growth. Addressing these challenges through robust security measures, user-friendly interfaces, and flexible pricing models will be crucial for sustained market expansion. The ongoing evolution of healthcare regulations and payment models will further shape the demand for PDM solutions, creating both opportunities and challenges for market participants. The focus on interoperability and data exchange standards will be vital in facilitating the seamless flow of provider data across the healthcare ecosystem.
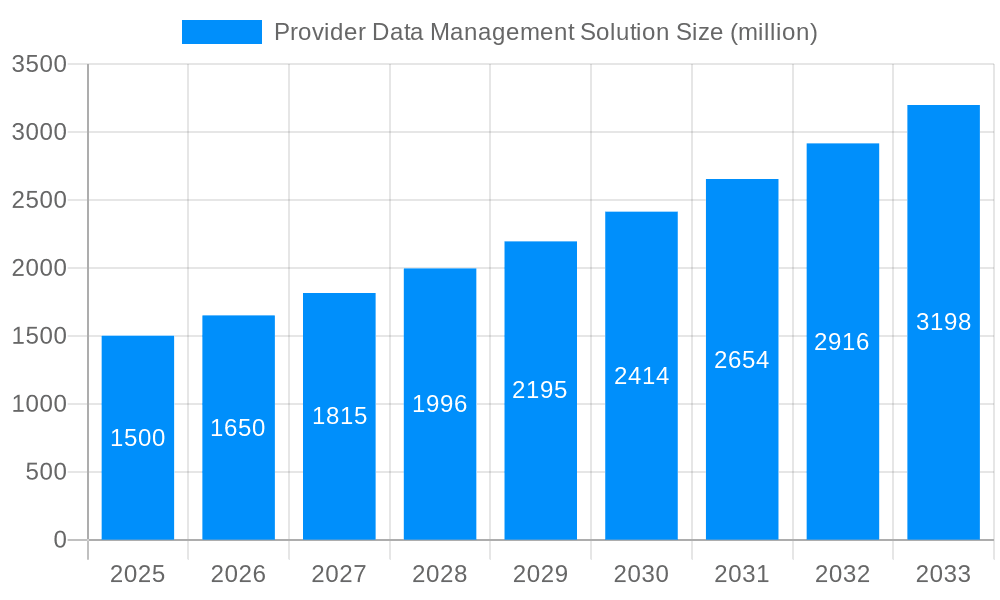

The provider data management (PDM) solution market is experiencing explosive growth, projected to reach multi-billion dollar valuations by 2033. This surge is fueled by the increasing complexity of healthcare data, stringent regulatory compliance requirements (like HIPAA), and a growing need for interoperability across disparate healthcare systems. The historical period (2019-2024) witnessed a steady climb in adoption, primarily driven by large enterprises seeking to streamline their operational workflows and enhance the accuracy of provider information. The estimated market value in 2025 is already substantial, exceeding several hundred million dollars, reflecting the significant investments made by both providers and technology companies. The forecast period (2025-2033) anticipates continued expansion, spurred by the accelerating adoption of cloud-based solutions and the rising demand for data-driven insights within the healthcare industry. This trend is particularly evident in the increasing utilization of advanced analytics for population health management and improved patient care coordination. The shift toward value-based care further accelerates the demand for robust PDM solutions, enabling providers to efficiently track performance metrics and optimize resource allocation. Furthermore, the growing recognition of the importance of accurate provider data for successful claims processing and revenue cycle management is a critical driver. This report analyzes the market landscape considering these trends, examining the key players, competitive strategies, and potential disruptions that may impact the market's trajectory over the next decade. The focus will be on understanding how different segments (cloud-based, web-based, large enterprises, SMEs) are contributing to this overall growth, offering valuable insights for both market participants and stakeholders. Finally, a comprehensive understanding of the regional variations in adoption rates will enhance our projections and provide a more nuanced picture of this dynamic market.
Several key factors are propelling the growth of the provider data management solution market. The increasing volume and complexity of healthcare data necessitate efficient management systems. Manual processes are becoming unsustainable, leading organizations to seek automated solutions capable of handling vast datasets, ensuring accuracy, and mitigating human error. Stringent regulatory compliance, primarily driven by HIPAA and other international regulations, mandates accurate and up-to-date provider data, making compliance a significant driver of PDM solution adoption. The shift towards value-based care necessitates precise data on provider performance and patient outcomes, driving the demand for analytical capabilities integrated within PDM solutions. Furthermore, improved interoperability between different healthcare systems is crucial for efficient care coordination and information exchange. PDM solutions facilitate data exchange, enhancing seamless communication between providers, payers, and patients. The rising adoption of cloud-based solutions offers scalability, cost-effectiveness, and enhanced accessibility, further fueling market growth. Lastly, the increasing focus on data-driven decision-making across healthcare organizations is driving the demand for PDM solutions equipped with robust analytics features, enabling stakeholders to gain valuable insights from their provider data to optimize operations and improve patient care.
Despite the significant growth potential, the provider data management solution market faces several challenges. Data integration remains a major hurdle, as healthcare systems often utilize disparate and incompatible technologies, making it difficult to consolidate data from multiple sources. Maintaining data accuracy and consistency is another significant challenge, requiring robust data validation and cleansing processes. Ensuring data security and privacy, particularly in light of increasing cyber threats and stringent regulations like HIPAA, necessitates significant investment in security infrastructure and compliance measures. The high initial investment cost associated with implementing PDM solutions can be a barrier for smaller healthcare providers and organizations with limited budgets. The need for skilled professionals to manage and interpret the vast amounts of data generated by these solutions presents a talent acquisition challenge. Furthermore, the continuous evolution of healthcare regulations and technological advancements require ongoing adaptation and updates of PDM solutions, representing an ongoing operational cost. Finally, addressing data governance issues and ensuring data quality across diverse healthcare settings remain key concerns that need to be addressed for the market to continue its trajectory of growth.
The North American market, particularly the United States, is expected to dominate the provider data management solution market during the forecast period (2025-2033). This dominance stems from several factors, including the advanced healthcare infrastructure, high adoption rate of technology, and stringent regulatory compliance requirements. The large number of healthcare providers and payers in the region, coupled with significant investments in healthcare IT, contribute to the market's rapid growth. Europe is also anticipated to show significant growth, driven by increasing digitization efforts across the region and growing adoption of electronic health records (EHRs). However, the pace of adoption might be slower compared to North America due to variations in healthcare systems and regulatory frameworks across different European countries. Focusing on the segment, the Cloud-Based solutions are poised for significant market dominance.
Cloud-based solutions: Offer scalability, cost-effectiveness, and enhanced accessibility, making them attractive to a wide range of healthcare organizations, from large enterprises to SMEs. The pay-as-you-go model minimizes upfront investments, and the flexible nature of cloud solutions allows for easy scaling as an organization's needs evolve. This flexibility is particularly beneficial in the dynamic healthcare landscape where data volumes and compliance requirements can change rapidly. Enhanced security features offered by reputable cloud providers further bolster their appeal. Cloud solutions offer greater interoperability, supporting seamless data exchange between different healthcare systems.
Large Enterprises: Large healthcare systems and provider networks are driving the adoption of sophisticated PDM solutions due to their ability to manage large volumes of provider data, enhance operational efficiency, and improve revenue cycle management. These organizations typically have the resources to invest in robust solutions, integrating them into their existing IT infrastructure. The potential for cost savings through improved efficiency and reduced errors makes such investments worthwhile.
The combined impact of these factors positions the North American market and the cloud-based segment as the dominant forces shaping the provider data management solution market in the coming years. The report further details regional variations in adoption rates and how the segment adoption varies across the various geographic locations.
Several factors are catalyzing growth in the provider data management solution industry. The increasing focus on interoperability and data exchange standards is driving the adoption of solutions that facilitate seamless data sharing between different healthcare systems. The growing adoption of cloud-based technologies offers scalability, cost-effectiveness, and improved data accessibility. Furthermore, rising investments in data analytics and artificial intelligence (AI) are enhancing the capabilities of PDM solutions, allowing for better insights and improved decision-making. Finally, stringent regulatory compliance requirements and the shift toward value-based care are compelling healthcare providers to adopt robust PDM solutions to ensure compliance and optimize care delivery.
This report provides a comprehensive overview of the provider data management solution market, covering key trends, driving forces, challenges, and growth opportunities. It analyzes market segments by type (cloud-based, web-based), application (large enterprises, SMEs), and geography. The report also profiles leading players in the market, including their strategies, market share, and competitive landscape. The detailed analysis provides valuable insights into the market dynamics, assisting stakeholders in making informed decisions regarding investments and future strategies in this rapidly expanding sector. The forecast period extending to 2033 offers a long-term perspective, enabling strategic planning and investment decisions.

| Aspects | Details |
|---|---|
| Study Period | 2020-2034 |
| Base Year | 2025 |
| Estimated Year | 2026 |
| Forecast Period | 2026-2034 |
| Historical Period | 2020-2025 |
| Growth Rate | CAGR of 5% from 2020-2034 |
| Segmentation |
|




Note*: In applicable scenarios
Primary Research
Secondary Research

Involves using different sources of information in order to increase the validity of a study
These sources are likely to be stakeholders in a program - participants, other researchers, program staff, other community members, and so on.
Then we put all data in single framework & apply various statistical tools to find out the dynamic on the market.
During the analysis stage, feedback from the stakeholder groups would be compared to determine areas of agreement as well as areas of divergence
The projected CAGR is approximately 5%.
Key companies in the market include Availity, Kyruus, LexisNexis, ApexonHealth, Knipper, CAQH, Andros, VerityStream, Simplify Healthcare, NextGate, Symplr, Change Healthcare, HealthEC, Perspecta, SKYGEN USA, .
The market segments include Type, Application.
The market size is estimated to be USD 1012 million as of 2022.
N/A
N/A
N/A
N/A
Pricing options include single-user, multi-user, and enterprise licenses priced at USD 4480.00, USD 6720.00, and USD 8960.00 respectively.
The market size is provided in terms of value, measured in million.
Yes, the market keyword associated with the report is "Provider Data Management Solution," which aids in identifying and referencing the specific market segment covered.
The pricing options vary based on user requirements and access needs. Individual users may opt for single-user licenses, while businesses requiring broader access may choose multi-user or enterprise licenses for cost-effective access to the report.
While the report offers comprehensive insights, it's advisable to review the specific contents or supplementary materials provided to ascertain if additional resources or data are available.
To stay informed about further developments, trends, and reports in the Provider Data Management Solution, consider subscribing to industry newsletters, following relevant companies and organizations, or regularly checking reputable industry news sources and publications.