1. What is the projected Compound Annual Growth Rate (CAGR) of the Healthcare Payer Analytics?
The projected CAGR is approximately 24.5%.
MR Forecast provides premium market intelligence on deep technologies that can cause a high level of disruption in the market within the next few years. When it comes to doing market viability analyses for technologies at very early phases of development, MR Forecast is second to none. What sets us apart is our set of market estimates based on secondary research data, which in turn gets validated through primary research by key companies in the target market and other stakeholders. It only covers technologies pertaining to Healthcare, IT, big data analysis, block chain technology, Artificial Intelligence (AI), Machine Learning (ML), Internet of Things (IoT), Energy & Power, Automobile, Agriculture, Electronics, Chemical & Materials, Machinery & Equipment's, Consumer Goods, and many others at MR Forecast. Market: The market section introduces the industry to readers, including an overview, business dynamics, competitive benchmarking, and firms' profiles. This enables readers to make decisions on market entry, expansion, and exit in certain nations, regions, or worldwide. Application: We give painstaking attention to the study of every product and technology, along with its use case and user categories, under our research solutions. From here on, the process delivers accurate market estimates and forecasts apart from the best and most meaningful insights.
Products generically come under this phrase and may imply any number of goods, components, materials, technology, or any combination thereof. Any business that wants to push an innovative agenda needs data on product definitions, pricing analysis, benchmarking and roadmaps on technology, demand analysis, and patents. Our research papers contain all that and much more in a depth that makes them incredibly actionable. Products broadly encompass a wide range of goods, components, materials, technologies, or any combination thereof. For businesses aiming to advance an innovative agenda, access to comprehensive data on product definitions, pricing analysis, benchmarking, technological roadmaps, demand analysis, and patents is essential. Our research papers provide in-depth insights into these areas and more, equipping organizations with actionable information that can drive strategic decision-making and enhance competitive positioning in the market.
 Healthcare Payer Analytics
Healthcare Payer AnalyticsHealthcare Payer Analytics by Type (Software, Hardware, Services), by Application (Clinical, Financial, Operational and Administrative), by North America (United States, Canada, Mexico), by South America (Brazil, Argentina, Rest of South America), by Europe (United Kingdom, Germany, France, Italy, Spain, Russia, Benelux, Nordics, Rest of Europe), by Middle East & Africa (Turkey, Israel, GCC, North Africa, South Africa, Rest of Middle East & Africa), by Asia Pacific (China, India, Japan, South Korea, ASEAN, Oceania, Rest of Asia Pacific) Forecast 2026-2034
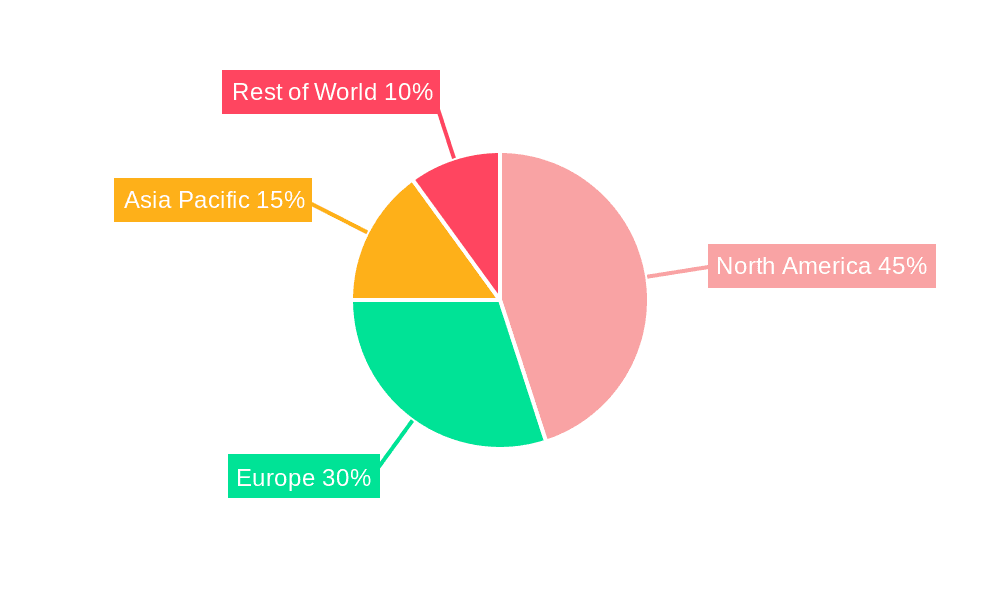
The healthcare payer analytics market is experiencing robust growth, driven by the increasing need for data-driven decision-making within the healthcare industry. The market's expansion is fueled by several key factors: the rising volume of healthcare data, the escalating pressure to reduce costs and improve operational efficiency, the demand for better risk management and fraud detection, and the growing adoption of value-based care models. Payer organizations are leveraging advanced analytics to gain insights into patient populations, optimize care pathways, predict healthcare utilization, and improve reimbursement accuracy. Software solutions are currently dominating the market, with a significant focus on clinical applications enabling precise risk stratification and proactive interventions. However, the market is witnessing a growing demand for integrated solutions combining software, hardware, and services to address the diverse analytical needs of payers. North America currently holds the largest market share, owing to the advanced healthcare infrastructure, high adoption rates of advanced technologies, and the presence of major market players. However, emerging economies in Asia-Pacific and other regions are showing significant potential for future growth due to increasing investments in healthcare infrastructure and the expanding digital health landscape.
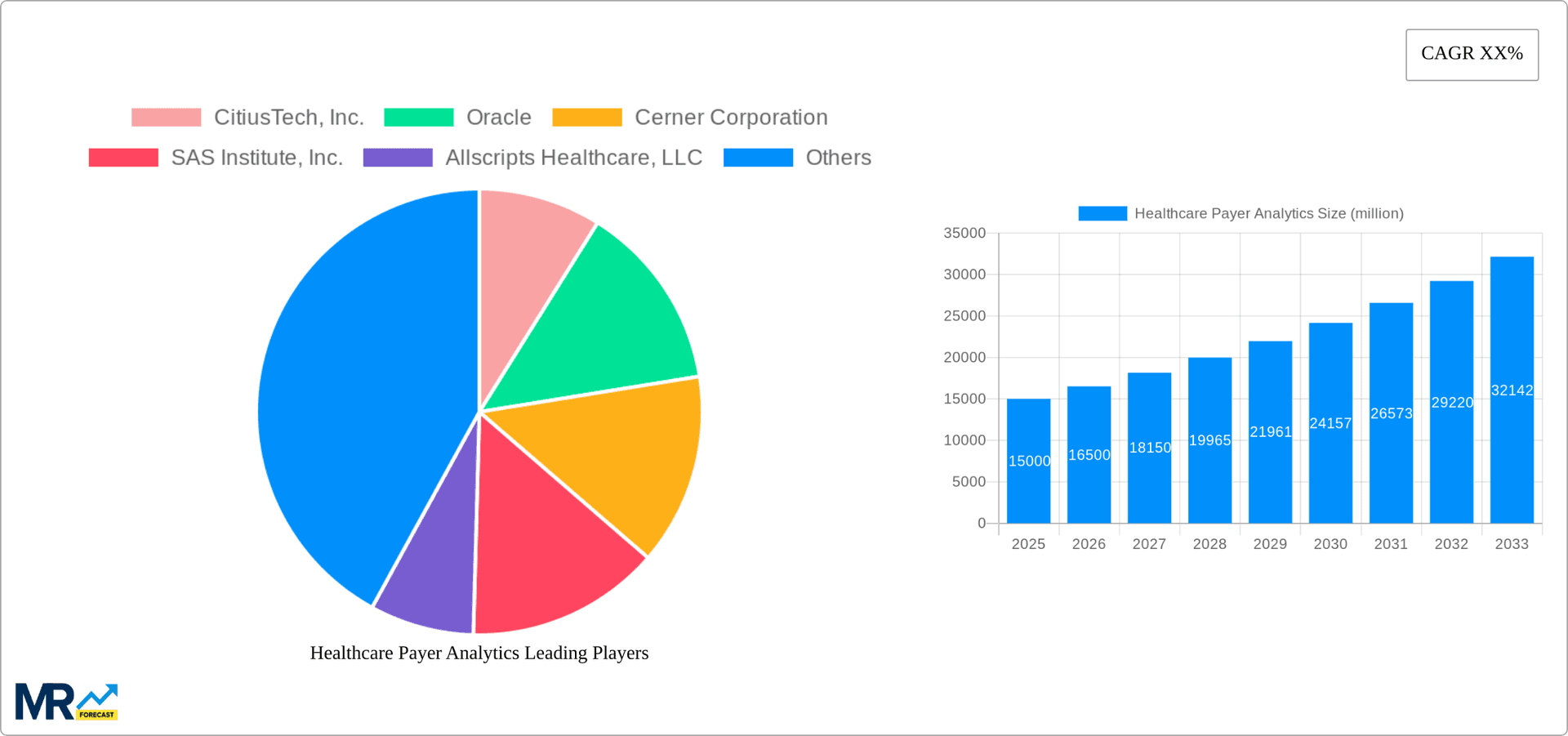

The market is further segmented by application into clinical, financial, operational, and administrative analytics. Clinical analytics helps payers understand patient populations, predict disease progression, and personalize care, while financial analytics focuses on cost optimization and revenue cycle management. Operational and administrative analytics aims to enhance efficiency in claims processing, member services, and other back-office functions. Key players in the market include established technology companies like Oracle and IBM, specialized healthcare analytics firms like CitiusTech and MedeAnalytics, and large healthcare providers with robust analytics capabilities like Optum. The competitive landscape is characterized by ongoing innovation, strategic partnerships, and mergers and acquisitions, driving further market consolidation and the development of more sophisticated analytics solutions. The long-term forecast indicates continued growth fueled by advancements in artificial intelligence, machine learning, and cloud computing, enabling more predictive and insightful analytics.


The healthcare payer analytics market is experiencing explosive growth, projected to reach multi-billion dollar valuations by 2033. This surge is driven by a confluence of factors, including the increasing volume and complexity of healthcare data, the escalating pressure to reduce costs and improve efficiency, and the rising demand for value-based care models. Key market insights reveal a strong preference for cloud-based solutions, enabling scalability and accessibility. The shift towards predictive analytics is also significant, allowing payers to proactively manage risks, personalize member experiences, and optimize resource allocation. Furthermore, the integration of artificial intelligence (AI) and machine learning (ML) is revolutionizing fraud detection, risk stratification, and treatment optimization, leading to substantial cost savings and improved patient outcomes. The market's evolution is characterized by a growing adoption of advanced analytics techniques, such as natural language processing (NLP) and deep learning, to extract actionable insights from unstructured data, like physician notes and clinical documentation. This improved data analysis significantly enhances care coordination and strengthens the provider-payer relationship. The historical period (2019-2024) showed significant adoption across the board, laying a robust foundation for the substantial growth expected during the forecast period (2025-2033). The estimated market size in 2025 demonstrates a crucial milestone in this upward trajectory, reflecting the consolidation of existing trends and the emergence of newer technologies. This report thoroughly analyzes these trends, providing critical insights for stakeholders seeking to navigate this dynamic market landscape. The base year for this analysis is 2025, allowing for a clear understanding of the current state and future projections.
Several key factors are fueling the rapid expansion of the healthcare payer analytics market. The increasing availability of large datasets from electronic health records (EHRs), claims data, and wearable devices provides rich raw material for advanced analytics. This data-driven approach allows payers to gain deeper insights into patient populations, identify high-risk individuals, and tailor interventions accordingly. Regulatory pressures, such as the push for value-based care and the emphasis on cost-effectiveness, are also significantly impacting the market. Payers are under immense pressure to demonstrate value and control costs, leading to increased investment in analytics solutions that can enhance efficiency and improve outcomes. Furthermore, technological advancements in areas like AI, ML, and big data technologies are enabling the development of more sophisticated and insightful analytical tools. These advancements are not just improving the accuracy and speed of analysis but also unlocking new opportunities for predictive modeling and proactive care management. Finally, the growing awareness among payers of the potential benefits of data-driven decision-making is creating a strong demand for analytics solutions. This demand is further amplified by the need to improve operational efficiency, reduce administrative costs, and enhance member satisfaction.
Despite the substantial growth potential, the healthcare payer analytics market faces certain challenges and restraints. Data interoperability remains a significant hurdle, with the lack of standardized data formats hindering seamless data integration and analysis across different systems. This challenge is amplified by the complexity of healthcare data, which often includes both structured and unstructured information from various sources. Another major challenge is data security and privacy. Protecting sensitive patient data is crucial, and stringent regulations like HIPAA necessitate robust security measures, adding to the complexity and cost of implementing analytics solutions. The lack of skilled professionals who can effectively interpret and utilize the insights generated by advanced analytics is also a significant constraint. The demand for data scientists, analysts, and other specialized professionals far surpasses the supply, creating a bottleneck in the market's growth. Furthermore, the high initial investment costs associated with implementing and maintaining sophisticated analytics infrastructure can be a barrier to entry for smaller payers, particularly in resource-constrained settings. Finally, the need for continuous updates and upgrades to keep pace with evolving technologies and regulatory changes adds to the overall financial burden.
The Software segment is poised to dominate the healthcare payer analytics market in the coming years. This is due to the increasing adoption of sophisticated software applications capable of handling large volumes of healthcare data and providing actionable insights.
North America is expected to remain a dominant player, driven by high technology adoption rates, the presence of major healthcare payers, and robust regulatory support for data-driven healthcare initiatives. The region's advanced healthcare infrastructure and significant investments in analytics solutions contribute to its leading market position.
Software Applications: The Financial application segment within the software category will experience significant growth due to the need for enhanced cost management, claims processing efficiency, and revenue cycle optimization. Precise cost estimations, timely payments, and improved financial forecasting are crucial for payers, driving adoption.
Software in Specific: Cloud-based analytics software will experience strong adoption, supported by increasing data volumes, improved scalability, and cost-effectiveness.
Geographical Diversification: While North America will likely lead, the market is seeing notable growth in other regions. Europe, for example, is making substantial investments in digital health infrastructure, stimulating the adoption of payer analytics solutions. Asia-Pacific countries are also showcasing robust growth, propelled by rising healthcare expenditure and increasing adoption of advanced technologies.
The overall market exhibits a strong focus on:
Improved efficiency in claims processing and payment: Payer analytics solutions significantly enhance these processes by automating tasks and minimizing human error, resulting in substantial cost savings.
Risk management and fraud detection: Predictive analytics empower payers to identify high-risk individuals and proactively address potential issues, effectively mitigating financial losses and ensuring compliance.
This dominance of software, specifically cloud-based financial applications, will continue to shape market dynamics and growth prospects throughout the forecast period. The interplay between these segments and regional growth patterns will dictate future investment strategies.
The healthcare payer analytics market is fueled by the convergence of several key growth catalysts. The increasing adoption of value-based care models necessitates precise measurement of outcomes and efficient resource allocation, driving demand for robust analytics solutions. Furthermore, the growing prevalence of chronic diseases and an aging population place greater pressure on healthcare systems, leading payers to proactively manage risks and personalize care, a task only achievable through sophisticated analytics. Advancements in artificial intelligence (AI) and machine learning (ML) are continuously enhancing the capabilities of these solutions, offering improved accuracy, efficiency, and predictive insights.
This report provides an in-depth analysis of the healthcare payer analytics market, offering valuable insights into market trends, growth drivers, challenges, and key players. It provides a comprehensive overview of the market landscape, including detailed segmentation and regional analysis, offering crucial data for strategic decision-making. The report's extensive forecast, spanning from 2025 to 2033, equips stakeholders with a clear understanding of the future market dynamics, allowing for informed investment and planning. The report incorporates historical data from 2019-2024 to establish a robust baseline for future projections.

| Aspects | Details |
|---|---|
| Study Period | 2020-2034 |
| Base Year | 2025 |
| Estimated Year | 2026 |
| Forecast Period | 2026-2034 |
| Historical Period | 2020-2025 |
| Growth Rate | CAGR of 24.5% from 2020-2034 |
| Segmentation |
|




Note*: In applicable scenarios
Primary Research
Secondary Research

Involves using different sources of information in order to increase the validity of a study
These sources are likely to be stakeholders in a program - participants, other researchers, program staff, other community members, and so on.
Then we put all data in single framework & apply various statistical tools to find out the dynamic on the market.
During the analysis stage, feedback from the stakeholder groups would be compared to determine areas of agreement as well as areas of divergence
The projected CAGR is approximately 24.5%.
Key companies in the market include CitiusTech, Inc., Oracle, Cerner Corporation, SAS Institute, Inc., Allscripts Healthcare, LLC, McKesson Corporation, MedeAnalytics, Inc., HMS, IBM, Optum, Inc., .
The market segments include Type, Application.
The market size is estimated to be USD XXX N/A as of 2022.
N/A
N/A
N/A
N/A
Pricing options include single-user, multi-user, and enterprise licenses priced at USD 3480.00, USD 5220.00, and USD 6960.00 respectively.
The market size is provided in terms of value, measured in N/A.
Yes, the market keyword associated with the report is "Healthcare Payer Analytics," which aids in identifying and referencing the specific market segment covered.
The pricing options vary based on user requirements and access needs. Individual users may opt for single-user licenses, while businesses requiring broader access may choose multi-user or enterprise licenses for cost-effective access to the report.
While the report offers comprehensive insights, it's advisable to review the specific contents or supplementary materials provided to ascertain if additional resources or data are available.
To stay informed about further developments, trends, and reports in the Healthcare Payer Analytics, consider subscribing to industry newsletters, following relevant companies and organizations, or regularly checking reputable industry news sources and publications.